An anal fistula is a tunnel that forms between the anal canal at the end of your colon and the skin around your bottom. This article gives an overview of anal fistulas.
A fistula is an abnormal tunnel between two organs in the body (such as the bowel and bladder). In an anal fistula a tunnel forms between the anal canal at the end of your colon and the skin around your anus (the part of your bottom where poo leaves).
They are also referred to as perianal fistulas, with peri meaning ‘around’.
Most anal fistulas develop after an anal abscess that hasn’t healed or drained away properly.
Anal abscesses can form when small glands inside the anus get clogged. This can cause an infection and an abscess can develop.
Certain things can make you more likely to develop an anal abscess or anal fistula. These include:
Less commonly anal fistulas can occur if you have ulcerative colitis and have had surgery to form an ileo-anal pouch.
One in every 2-4 people with an anal abscess go on to develop an anal fistula1.
Around a third of people with Crohn’s disease develop a fistula at some point in their life and around 3% of people with ulcerative colitis will get one2.
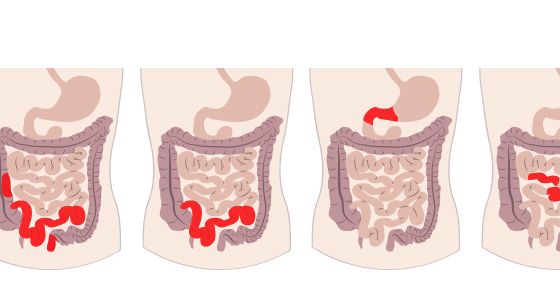
Anal fistulas can be a single tunnel (simple fistula) or branch off into several tunnels (complex fistula). Some fistulas may form through muscles in your bottom which can be responsible for controlling your bowels.
Anal fistulas are given different names depending on where they are in relation to parts of the anal sphincter (the muscle that controls our bowel movements). These are:
The most common type is intersphincteric and the least common is extraphincteric.
Some of the common symptoms of an anal fistula include:
If you have symptoms of an anal fistula you should speak to a doctor as soon as you can, especially if you know you’ve previously had an anal abscess.
This may be your general practitioner or a specialist consultant like a gastroenterologist if you are under their care for a condition such as Crohn’s disease.
The doctor will talk to you about your symptoms and any relevant medical history, such as if you have Crohn’s disease or have recently had a known anal abscess.
They should also carry out a physical examination which will involve looking at the area around your bottom and your anus. They may press the area to see if it’s sore or if a discharge comes out and insert a finger into your bottom (anus) to see if they can feel anything.
If it’s thought you have an anal fistula then you may be referred for more investigations. Some of these may be done under general anaesthetic and can include:
Anal fistulas rarely go away by themselves so treatment will likely be necessary.
If your fistula is caused as a result of Crohn’s disease or ulcerative colitis then your anal fistula may be treated using medication, surgery or a combination of both.
These medicines may include:
Some of the surgical options available include:
There aren’t many non-surgical options to treat an anal fistula. They currently include:
If an anal fistula is left untreated they can be very painful and can lead to a bacteria infection which can cause sepsis. Sepsis can be life-threatening.
Complications after anal fistula surgery can include:
Links from other sources used to create this article:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/anal-fistula
https://gutscharity.org.uk/advice-and-information/conditions/anal-fistulas/
https://fascrs.org/patients/diseases-and-conditions/a-z/abscess-and-fistula-expanded-information
https://111.wales.nhs.uk/Analfistula/
https://www.ncbi.nlm.nih.gov/books/NBK560657/
https://www.colorectalcentre.co.uk/abscess-fistula.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5716793/
https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-021-02078-9
https://www.cedars-sinai.org/health-library/diseases-and-conditions/f/fistula.html
https://nafc.org/bhealth-blog/8-most-common-questions-about-fistulas-answered/