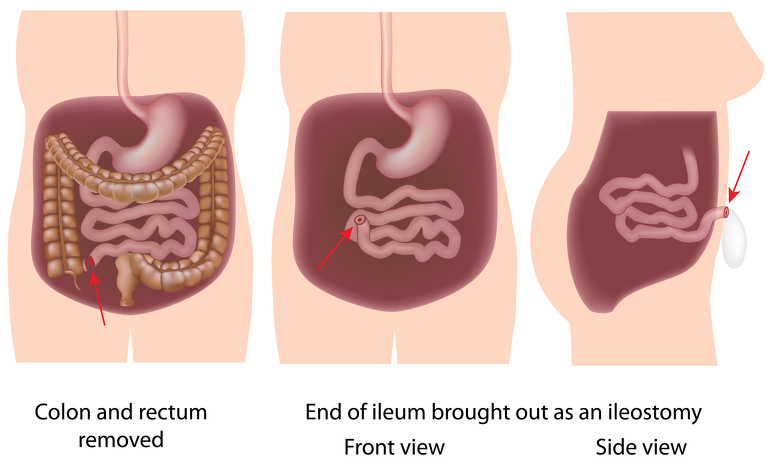
Pan-proctocolectomy surgery removes the entire colon, anal canal and rectum. It is mostly used to treat ulcerative colitis but is also used to treat types of Crohn’s disease which affect the colon - Crohn’s (granulomatous) colitis and ileocolitis. It is also known as total proctocolectomy.
If your inflammatory bowel disease (IBD) is not responding to other treatments - such as medication - and you have severe inflammation or damage to all, or part, of your large intestine (colon) and rectum then you may have a pan-proctocolectomy.
You may also have this surgery if your bowel perforates or you have bowel cancer or a very high chance of developing it.
The day before your surgery you will likely be asked to take a bowel preparation which will give you diarrhoea to clear the bowel of any faeces to make the operation easier. You may also need to follow a specific diet and avoid some medications.
Shortly before your surgery your blood pressure and breathing will be monitored and you will be prepared for theatre. You may be given medicine through a vein in your arm. Just before the surgery you will be given a general anaesthetic which will put you in a sleep-like state so that you won’t be aware of what’s happening.
Pan-Proctocolectomy surgery can be carried out either through open surgery or laparoscopic (keyhole) surgery. The type of surgery you receive will depend on your circumstances and the surgeon you have. It should be discussed with you prior to your operation.
Open surgery: An incision will be made along your abdomen to provide access to the colon for your surgeon. They will then identify the damaged section of the colon and remove it.
Laparoscopic surgery: Several small incisions (or ports) are made in the abdomen. A small camera is inserted through one of the ports to direct the surgeon to the colon. Surgical instruments are inserted through the other incisions and the colon is freed and then pulled through one of the ports. This type of surgery is meant to result in a quicker recovery time for the patient and also less scarring. In some cases the surgeon will discover during surgery that they need to convert to open surgery due to unforeseen circumstances.
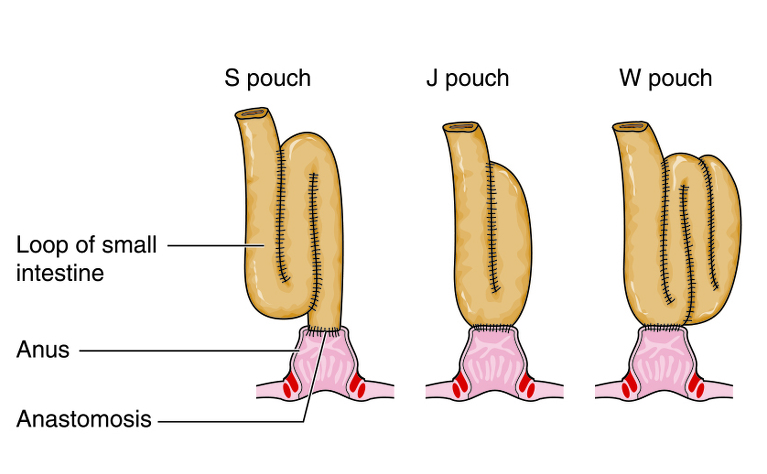
Once the surgeon has removed the colon and rectum the intestinal tract must be connected so you can pass stools.
This can be done in two different ways:
Once either of these procedures have been completed the surgeon will close the incision/s in your abdomen. How this is done depends on whether you received open or laparoscopic surgery. The wound in open surgery is often large and runs down the middle of the abdomen. In general this will be closed used clips which will then need to be removed around 10 days after surgery. The wounds in laparoscopic surgery are much smaller and often a special type of glue is used to fix them back together. This glue dries and falls off naturally. In both cases stitches may also be used - these can be dissolvable or may need removing around 10 days after surgery.
After your surgery you may need to stay in hospital for around a week until you regain normal bowel function. The length of your stay will also depend on whether you had open or laparoscopic surgery.
You may receive nutrition through an intravenous drip until your bowel has healed a little and you are able to drink more normally. You will probably be encouraged to eat and drink as soon as you feel able and will be encouraged to move around.
If your surgery involved the formation of a stoma then you will see an ostomy nurse who will teach you how to care for it.
It will probably take several weeks after leaving hospital for you to begin to feel better. You will probably be advised against any heavy lifting or strenuous physical activity and you may not be able to drive for a couple of weeks.
You may be recommended to follow a certain diet, or avoid certain foods, in the weeks immediately after surgery to aid healing.
There are risks associated with any abdominal operation and you should discuss the risks specific to you with your surgeon before the operation
There are different specific risks related to proctocolectomy and ileostomy or restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA). These are some of the general risks for the two: