Name: Edmund Murray
Year of Birth 1976
Lives: Glasgow, Scotland
Type of IBD: Pancolitis
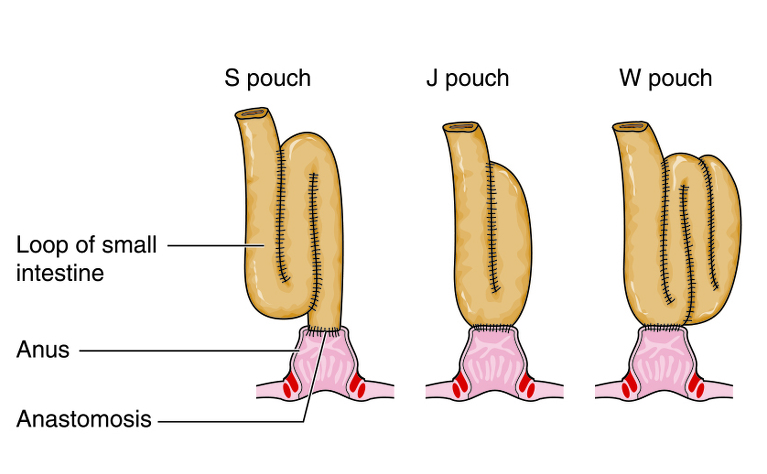
Details of Surgery: Restorative proctocolectomy with ileo-anal pouch (J-pouch) - in 2 stages. Stage 1 April 30, 2014, and stage 2 August 27, 2014
My body had become steroid dependant and the gastroenterologist told me there was a high risk of my colon exploding at some point in the future so I thought it would be better to donate my colon to medical research intact than wait for it to burst like a sausage.
My surgery was done in two stages: the first to remove my faulty colon and create the J-pouch (and a temporary stoma) and the second to reconnect everything back together.
Before my first operation I had to come off Azathioprine for two months as my immune system was so suppressed as a result of taking it for so long. I had an initial appointment with the surgeon, but he was running about 90 minutes late at his clinic that day so we agreed to have another meeting a couple of weeks later on his first appointment of the day so that we could discuss things fully without having to worry (too much) about the queue of people waiting.
The hospital (Gartnavel General in Glasgow) arranged for me to visit the high dependency unit (HDU) and IBD ward a week or so before the first operation to familiarise myself with them and meet some of the staff, including the stoma nurse who took me through what to expect with that side of things. I met again with the stoma nurse the day before to choose where the temporary stoma was going to be cited and then with the surgeon one final time to sign my consent form for the surgery. I also had various checks on my blood pressure, heart rate and so on to make sure I was going to be fine during the surgery. I was given some pre-operation “shakes” to drink at certain times in the run up to the surgery too.
Before each meeting, be it with the surgeon or the nurses, I made a list of questions I wanted to ask and when those were covered in the meeting I made notes as to what the answer was so that I had the answers down on paper for future reference.
In the build up to my second operation I met with the surgeon a couple of times to discuss how I was getting on and what was planned for the second time round. Since I had been in the HDU and IBD ward before I didn’t need to be shown around. I had a barium enema before being reconnected to make sure there were no problems with the J-pouch and I got to see what it looked like on the screens, although I also learnt not to believe a doctor who says 'this won’t hurt at all' as he used the endoscope.
The surgeon had a new assistant as part of the hospital’s surgical training programme so my second operation was put back by three weeks. The surgeon didn’t want to undertake complicated surgeries in their first few days of working together. When I was told this I was a bit disappointed at having to wait a bit longer as I was getting myself all psyched up for the whole surgery process again but I understood their reasons for the postponement.
On the day of the first surgery I was asked to arrive at the check-in for 7am since I was going to be the surgeon’s most difficult operation that day and he wanted to do it first. The hospital has a hotel right next door so I booked myself a room there the night before: partly so I didn’t have to travel to the hospital that early in the morning and also to have some peace and quiet on my own beforehand. I’m generally not one for having to get up at 05:30am but that day I was up out of bed before the alarm finished ringing. By that stage I had been waiting about three months for the operation so I was actually looking forward to getting it over and done with. I knocked back the two pre-op drinks as instructed, had a nice hot shower, got dressed and was waiting outside the operating theatre check-in at 06:50am.
Once they let me in one of the theatre nurses took me into a side room where she asked me a variety of questions to make sure I was aware of the surgery I was scheduled to have and why, gave me the hospital gown to wear, packed up my belongings to be taken up to the HDU once I was in theatre and then she stuck a big yellow sticker saying “similar name” on my notes (more on that later). I then went back into the waiting area in my very fetching hospital gown and then an anaesthetist came and spoke to me about being sedated. Shortly afterwards another anaesthetist came and spoke to me about whether I wanted to use an epidural which would apparently make things less painful once I came round compared to the anaesthetic they planned to use. Not having experienced either types of anaesthetic before I said I was happy to try this epidural if he felt it was the more appropriate.
I was then taken into a holding area on a hospital bed just outside all the operating theatres. After waiting there for a bit one of the nurses approached me and asked my name and so I told her. She looked puzzled and disappeared off somewhere. She came back with my notes and asked me to confirm my name and the operation I was expecting to have. It turned out she had been told a slightly different name for me and that someone with that name was booked for a different operation so she had to make completely sure the right person was going for the right operation. Then I realised why they had stuck a big yellow sticker saying “similar name” on my notes earlier.
I was then wheeled into another room outside the operating theatre itself where the anaesthetists were waiting with all their paraphernalia. They hooked me up to various things and then told me they were going to give the epidural and that I would feel a sharp prick in my lower back as they administered it. Sure enough it was quite painful and I remember thinking of some fairly industrial Glaswegian to describe the pain I felt. Then the lights went out.
For the second operation I went into the hospital the day before for another round of blood/heart tests and then another meeting with the surgeon to sign my life over to his hands again. As I was “only” being reconnected it was going to be his easiest operation of the ones he had on that day so I was to be his final operation. This meant I didn’t need to check in until mid-morning for my operation so this time my parents gave me a lift to the hospital and I checked in the same way as before, although this time without any confusion over similar names. This time round I also got a different anaesthetic, through a vein in my hand, which the anaesthetist told me would sting quite a bit which it certainly did before it kicked in and I keeled over.
When I came round after both my operations the first thing I remembered was to take the five deep breaths through the mask that I’d been told to do in the pre-operation meetings - I was impressed I was able to remember that.
As I was coming back round after the first operation the assistant surgeon came to speak to me and the first question I asked him was whether I was alive or not - which he was able to assure me I was. I then asked him if the operation had been a success and he told me they had been able to take out my faulty colon and create the J-pouch as well. I was pleased to hear this as the surgeons weren’t going to be sure if they could do this in one operation until they looked inside me due to the severity of my colitis. This meant I would, touch wood, need only one further operation. I then asked him if it was going to be OK to have the cat sit on me when I got home since I’d been sliced open right across the middle - although I was too taken aback by the look on his face that I didn’t actually listen to his response.
After a while I was wheeled up to the high dependency unit and passed into their care. The anaesthetic was starting to wear off and having had abdominal surgery I felt as if someone had welded a huge slab of metal onto my stomach. I also had seven different surgical drips and drains sticking out of various parts of my body and trying to find a position to lie in without those causing me discomfort was a challenge in itself.
I remember being given some jelly and ice cream to eat that evening and my parents came in to visit. I also remember being very disappointed when the attractive female nurse who had been looking after me since I’d been moved to HDU finished her shift and was replaced by a male nurse from Australia, although he was very pleasant.
At one point during that night the Australian chap was helping me move around a bit and between the two of us I moved my stomach area a bit too much for my liking. I then spent the next few minutes teaching him my wide repertoire of Glaswegian swear words so he decided to call the on-duty anaesthetist who came to the HDU and we decided to hook me up to some Fentanyl which I could take as and when necessary to help alleviate the pain.
After about 24 hours in the HDU I was transferred into the IBD ward for the rest of my recovery. However, I think as a result of the adrenaline and the anaesthetic leaving my system I started feeling worse and worse and it culminated with me asking the nurses on the Friday evening to help me sit up in my bed as I didn’t have the motivation to move myself. I had gone for a 10k run on my lunch break the day before my operation and I was utterly frustrated with myself at not being able to do anything that I had been able to do before. Completely irrational but that was just how my mind was working.
I managed to get a good night’s sleep on the Friday night and woke up about 6am on Saturday morning feeling as if someone had hit the reset button. I decided to get up and try to walk about, much to the surprise of the nurses who were in their hand-over meeting with the staff from the next shift and debating whether or not I should be transferred back to the HDU.
Part of the recovery process meant I was expected to walk a certain amount each day, with the distances getting longer every day. I was also to take several protein shakes a day but in order to get these I had to get up and walk to the nursing station to ask for them which was obviously a Machiavellian way of ensuring I was getting up and about. The HDU ward was also on the same floor as the IBD ward, albeit at the other end of the building, so I soon managed to be able to walk along to it, although my discreet enquiries led me to find out the shift pattern of the attractive female nurse who’d looked after me initially meant she wouldn’t be back on shift until after I was scheduled to be released, much to my disappointment.
Now I was getting more proficient at getting up and about I had plenty of visitors to keep me occupied. The stoma nurse came by several times to help me with changing bags, some physiotherapists came to make sure I was able to support myself properly while getting in and out of bed and to make sure I could get up and down stairs without difficulty since there are stairs leading up to the front door of our house and some junior doctors and medical students came to speak to me about my experiences of suffering from UC. I was also getting the various drips and drains taken out, although the rubber tube that was up my backside was the last to be removed, much to my annoyance as it was incredibly difficult to find a comfortable position to sit in while it was in place.
I was still finding it frustrating at not having the same mobility as I did before the operation but fortunately a sister from the chaplaincy centre visited the ward while on her rounds and she told me as we were chatting to be good to myself and celebrate every little improvement as a victory rather than seeing things as being different compared to how they were before.
I was due to be kept in for a week following the operation but by the 6th day I was spending large parts of my day wooing the ward sister so it was deemed I was well enough to be released back into the wild. There was a bit of a wait until all the paperwork was sorted out and all the necessary medication was brought up from the pharmacy, but eventually I managed to shuffle out the hospital to my parent’s car and they drove me home to start the next phase of my recovery.
When I came round after my second operation, after remembering to take the five deeps breaths I’d been taught, I noticed I was in the same recovery bay as the first time and that I had woken up at 2:50pm, which was the same time I came to after my first operation. The surgeon’s new assistant soon appeared and told me they had been able to staple my rebuilt insides back together using keyhole surgery through the hole where the stoma had been so they hadn’t needed to make any further incisions. He then said I would be able to go straight to the IBD ward to recover rather than the HDU since it had been such a routine operation.
I was dutifully wheeled up to the ward and I was able to phone my parents to let them know things had gone well. The surgeon’s assistant had phoned my parents after I’d come round following my first operation and my poor old mother got a massive fright when she heard it was a surgeon on the other end of the line because she thought for a few seconds he was phoning with some bad news. I made it up to the ward in time for the dinner round so I enjoyed a tuna sandwich and my parents came to visit.
Physically I felt a lot better and in much less pain than I did after the first operation but this one was obviously a lot less intrusive than before. I didn’t have any drips or drains hanging off me this time so once the anaesthetic wore off it wasn’t long before I was chasing after the nurses once again. I was also happy to be reconnected as I didn’t feel “complete” while I had parts of my insides sticking out of my body and glad that things seemed to be fine after both operations.
About 24 hours after my tuna sandwich it became apparent that it had worked its way through my system and it was time for it to come out the other end. The surgeon had put a strong emphasis on learning to “hold on” as long as possible to get the J-pouch to stretch and get the muscles in my sphincter used to keeping stuff in again so I did that as best I could but it had to come out at some point so after that was over I was glad to know my insides were working again.
I was supposed to be kept in for five days after this operation and the surgeon had said I could be allowed home on the fourth day. However, I was struggling to keep my balance due to the pain on my right hand side where I’d been operated on so the physiotherapists decided I should stay in until the fifth day to make sure I could keep myself upright without difficulties rather than releasing me a day early and me falling over at home and injuring myself. Eventually all the necessary paperwork was sorted and I was released back into the wild once more.
Over the days after getting home I spent a lot of time catching up on sleep and going out for walks to build up my strength. However, there were a couple of things that caused me problems in the period between my two operations. The first was that I had a problem with adhesions which was even more painful than anything I’d ever experienced before, including UC or the surgery itself. I was carted off to the local A&E in the back of an ambulance and admitted for four days while they cleared through my system.
Secondly, I was having all manner of problems getting the stoma bags to stay on despite help from the stoma nurse with trying to resolve this. It began to affect my decisions about going places as I was never quite sure if and when a bag would start leaking while I was out and about. Had my ileostomy been permanent I would have found this to be more of a problem but eventually we managed to find a combination of equipment that reduced this problem. Also, being a queasy person I didn’t really like seeing parts of my insides sticking out my body.
Again, after my second operation I had a problem with adhesions, this time while up in Dundee, which culminated in me decorating the carpet of the hotel I was staying in with half-digested breakfast. My colleagues managed to help me get back to Glasgow, although I did end up back in A&E, which at midnight on a Saturday is quite an eye-opener. Fortunately, I didn’t need admitted on this occasion but it still wasn’t a pleasant experience to go through again.
I needed to go my GP regularly to get my wound checked over as it healed. Fortunately the practice nurse is my first love (probably explains my thing for nurses) and had worked on the IBD ward for many years previously, although before I had been diagnosed, so I was more than happy to be paying her regular visits. It took a bit of time for the wound to heal as it was cited right where the waistband of my trousers goes and the rubbing as I moved about aggravated it until it finally healed. Other than that, it was a case of learning how my new insides worked, how long it took for certain foods to work their way through the system and what things could cause me problems.
I have had a couple of blockages since being reconnected but even though they were incredibly uncomfortable, to say the least, I looked at how and what I ate in the build up to them to try to make sure I don’t make the same mistakes again. I’ve also paid attention to what the symptoms are so that if they occur again I know what is coming and that I need to get myself back home and rest.
Having surgery was certainly the right decision in my case. Around 18 months after the second operation I am free from any UC symptoms, only need to pass solids around 5 times every 24 hours and can “hold on” for a couple of hours if need be. I take a sachet of probiotics every morning and I think once I started taking these they certainly helped my body process food better. However, these pit stops are not at regular points during the day as I hoped they might be and depend on what I have eaten the day before. I was hoping things might become a bit more routine after surgery, but that’s a reflection on my expectations rather than a criticism of the results themselves: I certainly don’t want my faulty colon back! I’m still getting myself out of the habit of going to a bathroom just because one is available - but having spent the best part of a decade doing so this habit is slightly difficult to break.
Since I don’t need to take any other medication my body feels a lot better for it, although I do worry about any side effects that may become apparent in the future as a result of taking so much medicine once I was diagnosed. I do occasionally wake up in the morning to find that I’ve had a “wet fart” while sleeping but I’ve not had any accidents since the surgery, either while awake or at night.
I do get quite gassy inside at various points during the day but at the moment I don’t quite trust myself to be able pass this gas out on its own without something else accompanying it. Maybe over time this is something that will improve as it can be quite uncomfortable at times, not to mention noisy as my insides bubble away like a witch’s cauldron.
The other big change I have noticed is a change in the way I feel fatigued. When I had my colon I was continually tired and walking about in a zombie-like haze. However, since my surgery I seem to be either switched on or off. Once I am able to get myself going for the day I am unstoppable: it’s just the getting started which can be a problem! However, since I am more awake than I was previously I am certainly thinking a lot more clearly than I did when I was spaced out.

