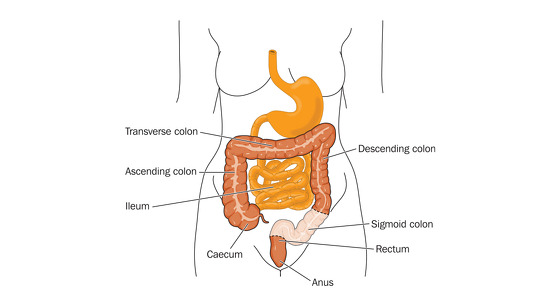
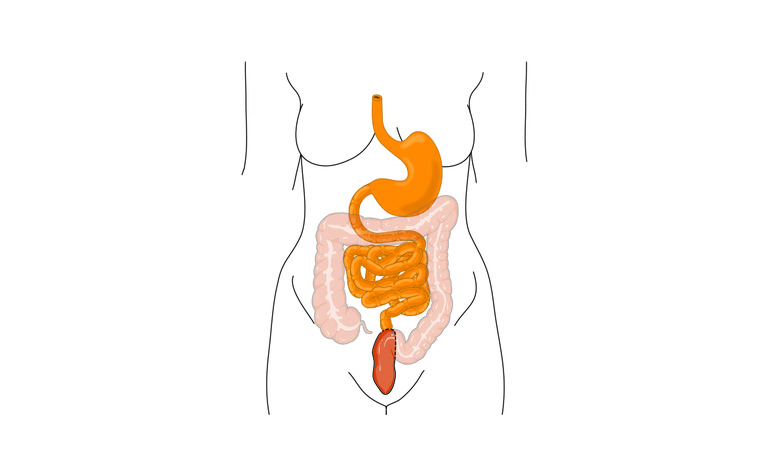
Colectomy surgery removes some, or all, of the colon (large intestine) which has been damaged due to Crohn's disease or ulcerative colitis (UC) - which are both forms of inflammatory bowel disease (IBD).
Other terms used to describe the surgery include colon resection surgery or hemicolectomy.
All forms of ulcerative colitis and Crohn’s disease affecting the large intestine (colon) - Crohn’s (granulomatous) colitis and ileocolitis.
If your IBD is not responding to other treatments - such as medication - and you have severe inflammation or damage to all, or part, of your large intestine (colon) then you may decide to have a colectomy. In a colectomy all, or part, of your colon is removed.
You may also have this surgery if your bowel perforates or you have bowel cancer or a very high chance of developing it.
There are a few different types of colectomy surgery and it’s important to understand which you are having. These are:
This article refers to the right and left hemicolectomy, transverse colectomy and total and partial colectomy surgery. There are separate articles on sigmoidectomy and proctocolectomy surgery.
The day before your surgery you will likely be asked to take a bowel preparation which will give you diarrhoea to clear the bowel of any faeces to make the operation easier. You may also need to follow a specific diet and avoid some medications.
Shortly before your surgery your blood pressure and breathing will be monitored and you will be prepared for theatre. You may be given medicine through a vein in your arm. Just before the surgery you will be given a general anesthetic which will put you in a sleep-like state so that you won’t be aware of what’s happening.
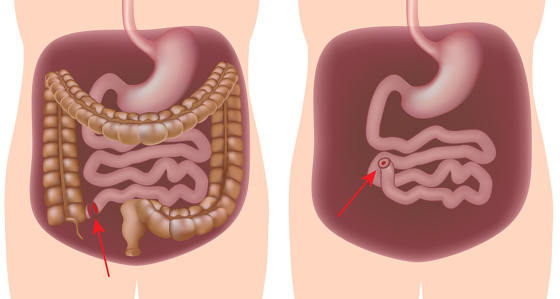
Colectomy surgery can be carried out either through open surgery or laparoscopic (keyhole) surgery. The type of surgery you receive will depend on your circumstances and the surgeon you have. It should be discussed with you prior to your operation.
Open surgery: An incision will be made along your abdomen to provide access to the colon for your surgeon. They will then identify the damaged section of the colon and remove it.
Laparoscopic surgery: Several small incisions (or ports) are made in the abdomen. A small camera is inserted through one of the ports to direct the surgeon to the colon. Surgical instruments are inserted through the other incisions and the damaged piece of the colon is pulled through one of the ports and operated on externally, before being reinserted. This type of surgery is meant to result in a quicker recovery time for the patient and also less scarring. In some cases the surgeon will discover during surgery that they need to convert to open surgery due to unforeseen circumstances.
Once the surgeon has removed the damaged parts of the colon the intestinal tract must be reconnected.
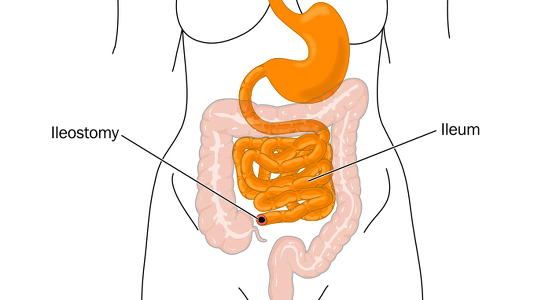
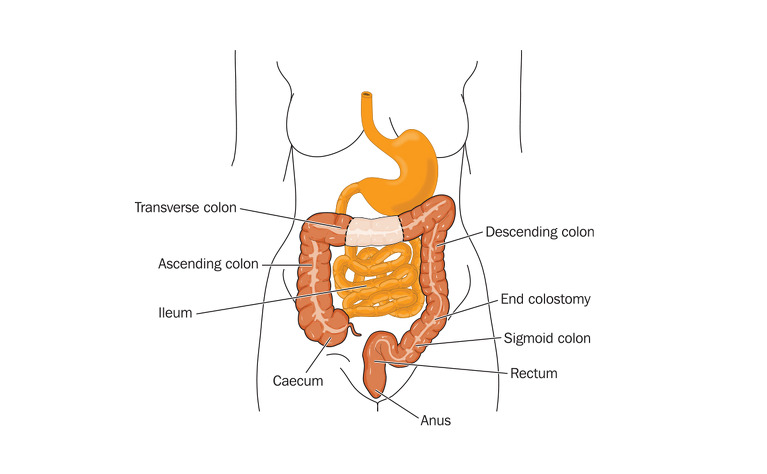
The surgeon then has several options:
How the surgeon closes the incision/s in your abdomen depends on whether you received open or laparoscopic surgery. The wound in open surgery is often large and runs down the middle of the abdomen. In general this will be closed using clips which will then need to be removed around 10 days after surgery. The wounds in laparoscopic surgery are much smaller and often a special type of glue is used to fix them back together. This glue dries and falls off naturally. In both cases stitches may also be used - these can be dissolvable or may need removing around 10 days after surgery.
After your surgery you may need to stay in hospital for around a week until you regain normal bowel function. The length of your stay will also depend on whether you had open or laparoscopic surgery.
You may receive nutrition through an intravenous drip until your bowel has healed a little and you are able to drink more normally. You will probably be encouraged to eat and drink as soon as you feel able and will be encouraged to move around.
If your surgery involved the formation of a stoma then you will see an ostomy nurse who will teach you how to care for it.
It will probably take several weeks after leaving hospital for you to begin to feel better. You will probably be advised against any heavy lifting or strenuous physical activity and you may not be able to drive for a couple of weeks.
You may be recommended to follow a certain diet, or avoid certain foods, in the weeks immediately after surgery to aid healing.