Pouchitis is inflammation that can occur in a surgically created pouch after having your large intestine removed.
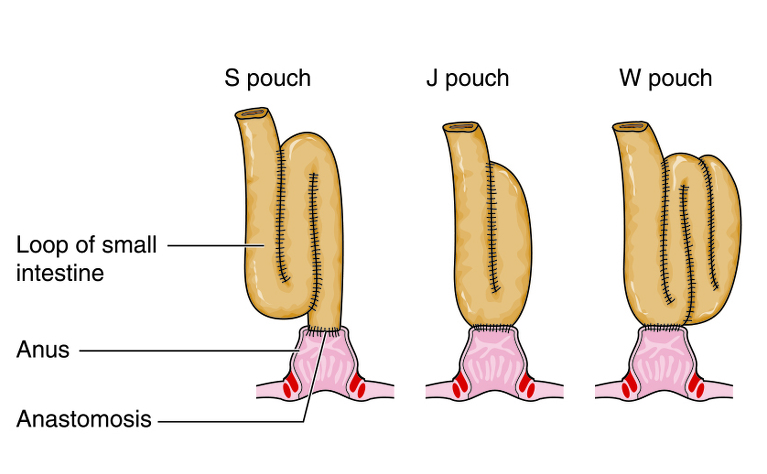
Pouchitis is inflammation of an ileal pouch (often referred to as J-pouch). It can only occur in people who have had surgery to remove their large intestine and rectum and form a pouch out of the end of their small intestine which is attached to the anus. This operation is called a restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA).
Symptoms of pouchitis may include:

Pouchitis is thought to be fairly common in people with an ileal pouch. It is believed up to 45% of people with a J-pouch will experience pouchitis in the 10 years after their operation, with 15% 1 year after and 33% 5 years after1,2. 50% of patients with a pouch are thought to experience pouchitis as some point3.
It isn’t known exactly what causes pouchitis but it tends to occur in people who have ulcerative colitis or another form of colitis (such as indeterminate colitis).
Your doctor may carry out an endoscopy and consider it along with your symptoms to diagnose pouchitis.
The first treatment usually tried on people with pouchitis is a 2 week course of antibiotics. This is often successful for people who haven’t had pouchitis before, however it can return at a later date. Pouchitis can become resistant to antibiotics. In these cases the pouch may be removed and a stoma created or a permanent diversion using another part of the small bowel may be carried out.
Probiotic treatment has shown to have some effectiveness and some doctor prescribe probiotics at the same time as taking antibiotics to repopulate your gut with good bacteria.
Doctors may also try using corticosteroids, immunosuppressants or biologic medications, though these haven’t been tested for use in people with pouchitis.
You may also be advised to make some changes to your diet to assist in relieving symptoms.
Severe cases of pouchitis can cause:
Severe cases of pouchitis, or recurrent cases, may results in the pouch needing to be removed.
Diagnosis and management of pouchitis. Uma Mahadevan, William J. Sandborn. Gastroenterology, May 2003, olume 124, Issue 6, Pages 1636‐1650 http://www.gastrojournal.org/article/S0016-5085(03)00325-1/fulltext?referrer=https%3A%2F%2Fen.wikipedia.org%2F
Pouchitis after ileal pouch-anal anastomosis for ulcerative colitis occurs with increased frequency in patients with associated primary sclerosing cholangitis. C Penna, R Dozois, W Tremaine, W Sandborn, N LaRusso, C Schleck, D Ilstrup. Gut BMJ Journal, Volume 38, Issue 2. http://gut.bmj.com/content/38/2/234