Perianal Crohn's is a form of Crohn's disease which causes inflammation around the anus.
Perianal Crohn’s disease is a form of Crohn’s disease which causes inflammation around the anus. It can occur on its own or at the same time as other forms of Crohn's disease which cause inflammation in other parts of the digestive system.
Perianal Crohn’s affects up to a third of people with Crohn’s disease. It is a life-long chronic condition which cannot currently be cured and is part of a group of conditions known as inflammatory bowel disease (IBD).
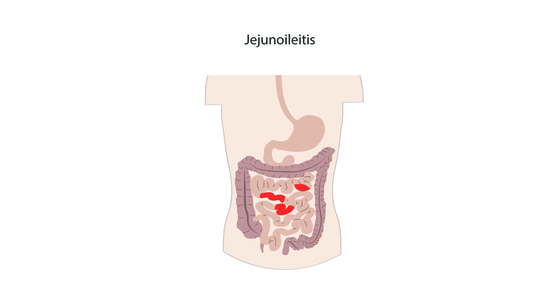
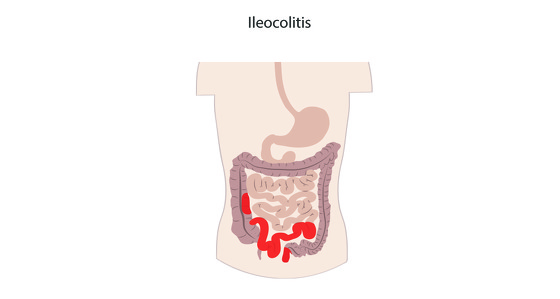
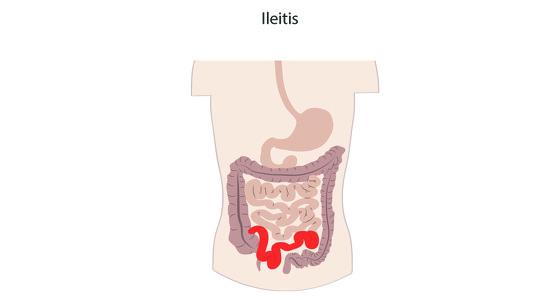
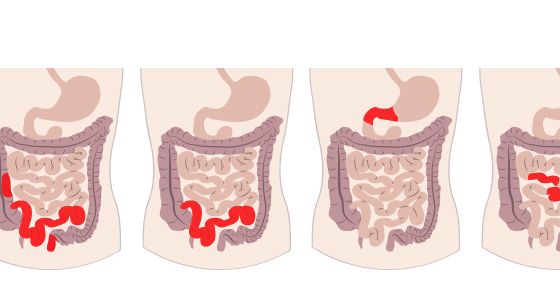
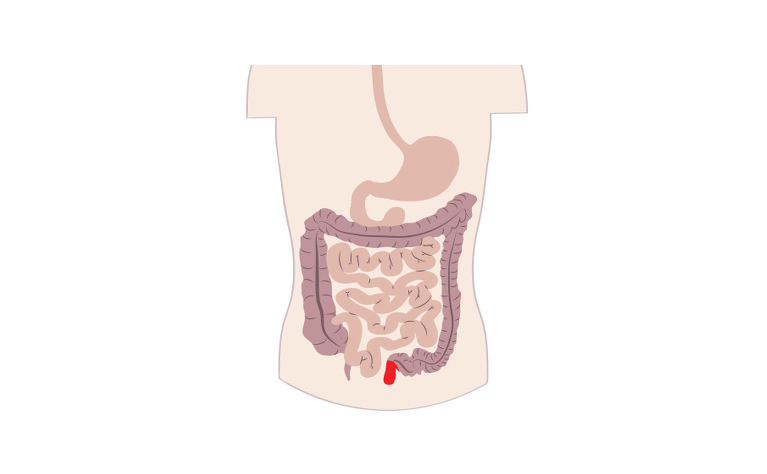
Crohn’s disease causes inflammation in the gastrointestinal (GI) tract. It most commonly affects the small intestine and the beginning of the large intestine, however it can affect any part of the GI tract from the mouth to the anus.
Crohn’s disease affects the entire thickness of the digestive tract wall and may also skip areas - meaning you could have inflammation near your mouth and also in your small bowel but no where in between.
It is common for people with Crohn’s disease to be diagnosed with more than one type of the condition if inflammation is present in several places in the GI tract.
Typical symptoms of perianal Crohn's include:
Treatments currently include medication and surgery. Some people have severely inflamed or damaged parts of their bowels surgically removed. This can reduce or eliminate the symptoms, however it does not get rid of the disease and there is a risk that it will return to another area of the GI tract in the future.
Some people also make adjustments to their diet and lifestyle to support their medical treatment - such as exercise, improving quality of sleep, reducing stress.