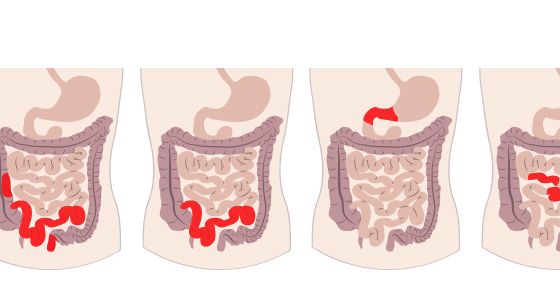
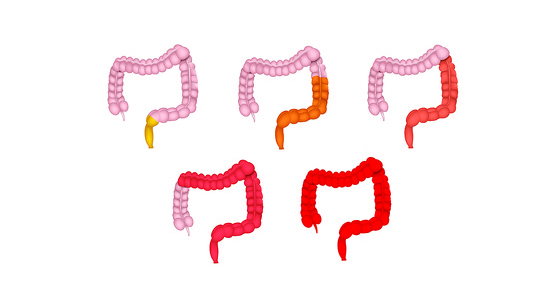
Methotrexate belongs to a group of medicines called immunosuppressants. It works on inflammatory bowel disease (IBD) by reducing the activity of the immune system which, in turn, reduces inflammation in the bowel.
Methotrexate was first used in 1947 to treat leukaemia and other forms of cancer but in the 1980s it was used in much lower doses to treat conditions such as rheumatoid arthritis and psoriasis and has gone on to be used in treating Crohn’s disease and ulcerative colitis.
Methotrexate is not licensed for use in treating IBD in the UK, however it has safely been used for more than 20 years to help induce and maintain remission in Crohn’s disease and, less commonly, ulcerative colitis. It is usually prescribed to people who have recurrent flares which need steroids to control them and people who haven’t responded to other medications (such as azathioprine).
It is known under several different brand names including Trexall, rheumatrex and may be referred to as just MTX.
Methotrexate is taken once a week either by tablet or injection.
Tablets
These should be taken after food on the same day each week. The tablets come in two doses - 2.5mg and 10mg. When you pick up a new prescription of your tablets you should always make sure that you have the right dosage to prevent overdosing.
Injection
There are two types of injection for methotrexate - subcutaneous (under the skin) and intra-muscular (into the muscle). A nurse at a clinic may administer the injections or you may be trained to do them yourself at home. The injections should be carried out on the same day each week.
It can take up to three months to work and therefore you may be given other medication to take during this time to help control your IBD. If methotrexate is effective for you then you may take it for several years, or as long as you can tolerate it.
You may also be prescribed folic acid to take at the same time as methotrexate can cause you to develop levels of folate that are lower than normal. The folic acid tablets also help your body to cope with the medication and may reduce some of the side effects.
There are some medications that can interact with methotrexate so you should inform your doctor about any medications or other remedies, vitamins or complementary therapies you are taking. You should be particularly cautious with antibiotics such as co-trimoxazole and trimethoprim and non-steroidal anti-inflammatory medications like ibuprofen.
Some doctors prescribe methotrexate to be taken at the same time as biologic medications and this is safe to do so.
Oral contraceptives can be taken at the same time as methotrexate.
As with any medication there may be some undesirable effects while taking it. All the potential side effects will be listed in the patient information leaflet which accompanies your medication. Common side effects of taking methotrexate can include:
You should not receive any live vaccines (measles, mumps, rubella ie MMR, chickenpox, oral polio, BCG, oral typhoid and yellow fever) while taking methotrexate. The flu vaccine injection is safe, but the nasal version for children is not. You should also speak to your doctor if anyone you are in contact with is due to have a live vaccine as it may not be safe for you to be around them afterwards.