Having inflammatory bowel disease can sometimes lead to skin problems too. Find out more in this article….
Skin issues can affect people with inflammatory bowel disease (IBD) (such as Crohn’s disease and ulcerative colitis). A recent study1 reported almost one third of the patients with IBD develop skin conditions related to their disease or its treatment. The most common skin condition in patients with ulcerative colitis (UC) was psoriasis, and erythema nodosum in patients with Crohn’s disease. Skin conditions were significantly more prevalent in those patients with severe UC or Crohn’s disease.
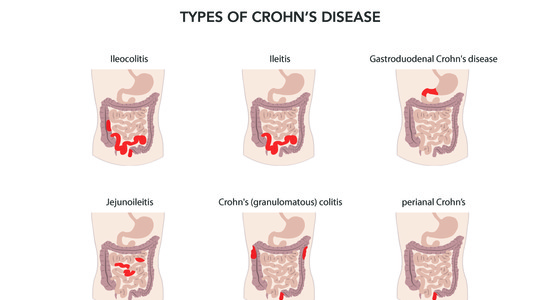
Some of the skin issues may be caused by inflammation in your body, especially during a flare, whilst some other skin issues could be linked to the medication you take to treat your IBD. A 2015 study2 concluded that ‘IBD is a systemic disease, and EIM (extra-intestinal manifestations) are the proof that IBD is not only limited to the gut’. You can experience symptoms that affect areas other than the digestive tract. In particular with Crohn’s disease EMIs may occur in up to 40% of patients, and disorders of the skin are among the most common.3
Malnutrition, where there’s a lack of sufficient nutrients in your body and vitamin and mineral deficiencies may also have an affect on your skin. For example:
Zinc deficiency - can cause red patches or plaques that may also have pustules
Iron deficiency - can cause red, cracked patches at the corners of the mouth
Vitamin C deficiency - can cause bleeding under the skin, which causes bruise-like spots to appear
Some skin issues may occur prior to a diagnosis of IBD. In up to one quarter of patients involved in the study ‘Skin Manifestations of Inflammatory Bowel Disease’4, EIMs presented before an IBD diagnosis was established. Skin conditions may therefore instigate further investigations especially if accompanied with bowel problems.
Other possible explanations for skin manifestations in IBD include genetic abnormalities, immune dysfunction and impairments in gut microbiota. However, more research is needed to further determine the links between IBD and skin conditions.
There are several skin conditions that are associated with having IBD, some common, some more rare. We’ve looked at some of those conditions here.
Pyoderma gangrenosum is another common skin issue associated with IBD. It can often happen during a flare. It usually appears on your ankles and shins, but may also develop on your arms. It begins as a cluster of small blisters that can spread and combine to create deep, sometimes very painful ulcers. It can cause scarring. It is important to keep the ulcers clean to avoid infection. High doses of corticosteroids may be prescribed as well as pain medication for the ulcers depending on its severity.

Hives are a red, often itchy skin rash that can occur on any part of your body. They may appear as a reaction to your IBD medication. Contact your doctor to discuss alternatives if you start a medication and you get persistent hives.


Psoriasis is an autoimmune condition, which presents as red, flaky patches on the skin that form white or silver-looking scales. It happens when the immune system goes into overdrive and causes skin cells to multiply too quickly. These extra cells build up on the skin. It is more common in Crohn’s disease. Treatment may include topical corticosteroids.
The findings from a study5 in 2018 suggest that psoriasis is significantly associated with IBD. Presenting with psoriasis and simultaneous bowel problems may therefore prompt investigation into an IBD diagnosis.


A much rarer skin manifestation is Sweet’s syndrome, which is linked to active IBD flares. It starts as small, tender, red or purple bumps that spread into painful clusters, usually on your upper body, neck or face. It may be accompanied by headaches, body pain, and a general feeling of being unwell. The bumps may appear black or brown on darker skin tones and red on lighter skin. The bumps may go away on their own but recurrence is common and may leave scars. The main treatment for Sweet’s syndrome is corticosteroids, either injected or in tablet form.

PPV refers to two skin conditions; pyodermatitis vegetans - a rash of red pustules, which can rupture and form raised scaly patches of skin and occurs in the skin folds of your armpit or groin; and pyostomatitis vegetans - where the pustules form in your mouth. These linked conditions are associated with UC. As with some other skin conditions, it may pre-date the onset of UC, which may alert your doctor to consider the possibility of an IBD diagnosis. PPV has been identified as having a correlation with underlying bowel disease activity6. Oral corticosteroids are thought to be the best treatment option.

In most mild cases of leukocytoclastic vasculitis, supportive measures can be effective to treat it e.g leg elevation, rest, compression stockings, and antihistamines. In more severe cases a 4-6 week dose of corticosteroids may be prescribed.
Acrodermatitis enteropathica appears as a flaky skin rash or blisters usually found on your hands, face, feet or genitals and is caused by a zinc deficiency. If you experience ongoing diarrhoea with your IBD, you may be losing zinc through your poo. Taking a zinc supplement should help alleviate the rash. Always speak to your doctor before taking any supplements.
Most skin issues associated with IBD are best treated by managing the IBD as much as possible, as many of these issues can coincide with being in a flare. If you do develop a rash or skin condition you may be prescribed corticosteroids to help with the inflammation that often causes the skin issues. For the rash itself, antibiotic ointment or pain medication may be prescribed to help alleviate the symptoms. Topical corticosteroids may also be prescribed.
Depending on the type of skin condition you have will determine the course of treatment. Potential treatments include:
Corticosteroids - oral, injected or topical
Immunosuppressive drugs, such as methotrexate or azathioprine
Anti-inflammatory medications, such as sulfasalazine
Anti-TNF biologics, such as infliximab or adalimumab
Antibiotics
If a particular medication is thought to be causing the skin condition, you may be advised to discontinue taking it. If a vitamin or mineral deficiency is thought to be the cause, your doctor may suggest you take vitamin or mineral supplements.
If you do experience an IBD associated skin condition, keep the area clean to prevent infections and see your doctor or IBD nurse or team for further advice or treatment, particularly if it covers a large area, has spread quickly, is painful, occurs with a fever or you have blisters or fluid drainage.
Here are some general tips for dealing with skin conditions, for more specific advice, please contact your doctor:
Patch test before using new cosmetics and hair products to check for irritation. Apply a small amount of the product to your skin and leave it on to see if a reaction develops. The American Academy of Dermatology (AAD) has advice on performing patch tests at home
Do not apply cosmetics to open sores
Avoid irritants such as soaps, bubble bath, detergents and any fabrics that seem to irritate. Cotton clothing is usually comfortable for people with skin conditions
If your skin condition is itchy, try not to scratch it (easier said than done!). Keep your nails short to limit any damage done to the skin by scratching
Try not to pick at a rash or scabs - it can make the condition worse, cause more discomfort and itching and lead to infections
1.Jonaityte, I.R, Kiudelis, G, Valiukeviciene, S, Kupcinskas, J, JonaitisProf., L. Skin lesions among consecutive Inflammatory bowel disease patients in outpatient setting. P866
2. Stephan R. Vavricka, MD, Alain Schoepfer, MD, Michael Scharl, MD, Peter L. Lakatos, MD, Alexander Navarini, MD, Gerhard Rogler, MD. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflammatory Bowel Diseases, Volume 21, Issue 8, 1 August 2015, Pages 1982–1992, https://doi.org/10.1097/MIB.0000000000000392
3. AG Gravina, A Federico, E Ruocco, A Lo Schiavo, F Romano, A Miranda, D Sgambato, M Dallio, V Ruocco, C Loguercio, and M Romano. Crohn’s disease and skin. PMCID: PMC4804366 DOI: 10.1177/2050640615597835
4. Thomas Greuter, Alexander Navarini, Stephan R Vavricka.Skin Manifestations of Inflammatory Bowel Disease PMID: 28643285 DOI: 10.1007/s12016-017-8617-4
5.Yun Fu, MD, Cheng-Han Lee, MD, Ching-Chi Chi, MD, MMS, DPhil. Association of Psoriasis With Inflammatory Bowel Disease AMA Dermatol. 2018;154(12):1417-1423. doi:10.1001/jamadermatol.2018.3631
6. Brian L. Huang, Stephanie Chandra, David Quan Shih. Skin Manifestations of Inflammatory Bowel Disease. PMCID: PMC3273725 DOI: 10.3389/fphys.2012.00013