Bowel cancer refers to cancer that starts in the large bowel. It is one of the most common types of cancer diagnosed in the UK. According to Bowel Cancer UK 1 in 15 men and 1 in 18 women will be diagnosed with bowel cancer during their lifetime1. The majority of these people are aged over 50, however it can affect anyone of any age.
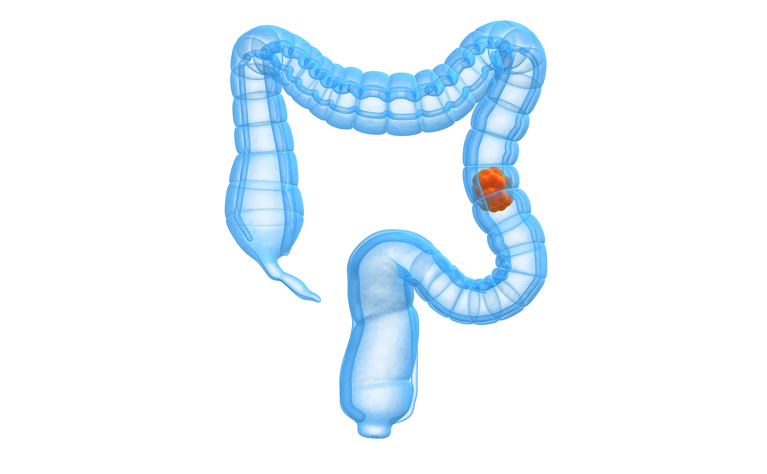
Bowel cancer is also referred to as colorectal cancer, colon cancer or rectal cancer (depending on where the cancer is located). Most cases of bowel cancer develop from pre-cancerous growths, called polyps - although not all polyps develop into cancer.
People with inflammatory bowel disease (IBD) can be at increased risk of developing bowel (colon) cancer than the general population. The majority of research that has been done looks at the link between ulcerative colitis (UC) and bowel cancer, but some research has shown that people with Crohn’s disease can be at risk too.
The main risk factors are:
There are also other risk factors which can increase anyone’s risk of developing bowel cancer. These include:
It’s important to remember that most people with IBD will not develop bowel cancer - but it’s important to be aware of your risk.
For people with ulcerative colitis the risk of bowel cancer only increases once you have had symptoms of the disease for 8-10 years. It also depends on how much of your bowel is affected. If UC affects the whole colon then your risk appears to be greater than if it just affects a small amount. If you just have UC in your rectum (proctitis) then your risk is little or no greater than for the general population.
There is also a genetic link and if a family member has had bowel cancer then you may be at even greater risk. You may also be at a higher risk if you have a liver condition called primary sclerosing cholangitis (PSC).
Your degree of risk will be related to the amount of inflammation that can be seen - the more inflammation, the more risk - and the amount of time you have had ulcerative colitis for.
Research has shown various risk increases, but a large meta study of all previous research has shown that risk increases for ulcerative colitis (irrespective of where your disease is located)2 are:
The general population has a lifetime risk of around 4.5% of developing bowel cancer.
People with Crohn’s disease in their colon (Crohn’s colitis) have a higher risk of developing bowel cancer. Studies show varying results as to the risk of bowel cancer for people with Crohn’s disease - ranging from 2-3 times to 6 times that of the general population3. The risk after 20 years of Crohn’s disease is reported as being in the region of 7%3, which is similar to the risk in people with ulcerative colitis after 20 years (8%).
Bowel cancer can also develop in the small intestine, though it is much rarer. It is thought only around 2% of people with Crohn’s disease in the small bowel develop cancer in this area4.
If you have had surgery to remove your colon and have an end ileostomy, but still have a rectal stump you can develop cancer in your stump. Studies have found that 1 in 48 ulcerative colitis patients with a stump may develop rectal cancer at anytime after colectomy5.
The overall risk of developing cancer in a j-pouch following ileal pouch-anal anastomosis (IPAA) surgery is very low. It is thought around 1 in 200 ulcerative colitis patients (0.5%) may develop pouch cancer any time after their surgery. Three studies have shown that after 10 years 0.9% developed pouch cancer and after 20 years 2.7% developed pouch cancer5.
Studies of ulcerative colitis patients who have undergone colectomy and ileorectal anastomosis (IRA) surgery have found that 1 in 42 (2.4%) patients may develop rectal cancer anytime after the surgery5. After 10 years 2% developed rectal cancer (1 study) and after 20 years 14%, these two figures are only based on one study5.
The main symptoms of bowel cancer are very similar to common symptoms of IBD.
They are:
Because it can be difficult to distinguish between IBD and bowel cancer symptoms it’s really important that you attend any screening or colonoscopies when asked by your doctor. This is especially important the longer you have had IBD for.
Screening for bowel cancer in people with IBD in their colon usually begins 8-10 years after onset of the disease.
Many people with IBD are found to have polyps in their bowel when they are undergoing a routine monitoring colonoscopy for their IBD. A polyp is a small growth on the inner lining of the bowel. They often don’t cause any symptoms, so many people are unaware they have them. Bowel cancer can develop from polyps, however they don’t usually turn into cancer.
If polyps are found during a colonoscopy your doctor may remove them during the procedure and send them off to be tested to see if there is any cancerous change in the polyp.
It’s impossible to change some of the things which put you at an increased risk of bowel cancer (such as your genes or having IBD), but there are some lifestyle factors which are thought to place anyone at a greater risk. Making some healthy lifestyle changes can help to mitigate against these risks. They include: