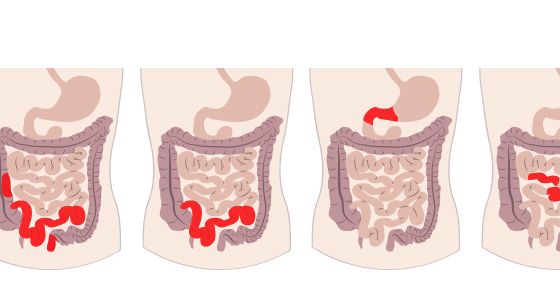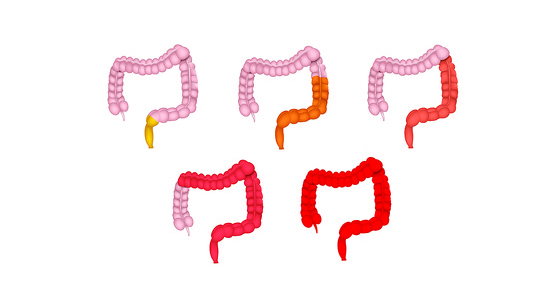
Microscopic colitis is a chronic, lifelong condition which is part of a group of conditions known as inflammatory bowel disease (IBD). It causes inflammation of the gastrointestinal tract (gut). This inflammation occurs in the colon (large intestine) and rectum. There are two main types of microscopic colitis - lymphocytic colitis and collagenous colitis - however they are very similar.
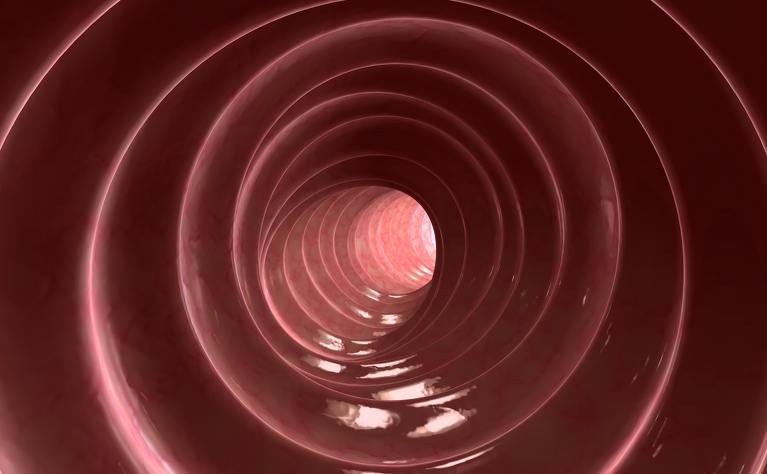
To the eye the lining of the colon may appear normal, however under a microscope changes to the bowel lining can be seen. The main symptom of microscopic colitis is watery diarrhoea (without blood).
The other types of IBD include ulcerative colitis (UC) and Crohn’s disease.
It is thought to be an autoimmune condition.
There is no known cure for microscopic colitis and is generally treated with medication and lifestyle changes - such as diet, exercise and reducing stress.
Some people with microscopic colitis do have surgery to remove parts of their colon and rectum which are affected, but this is rare.
Some of the common symptoms of microscopic colitis include:
There are two types of microscopic colitis - lymphocytic colitis and collagenous colitis. The symptoms and treatment are very similar, however they look very different under a microscope.
Lymphocytic colitis
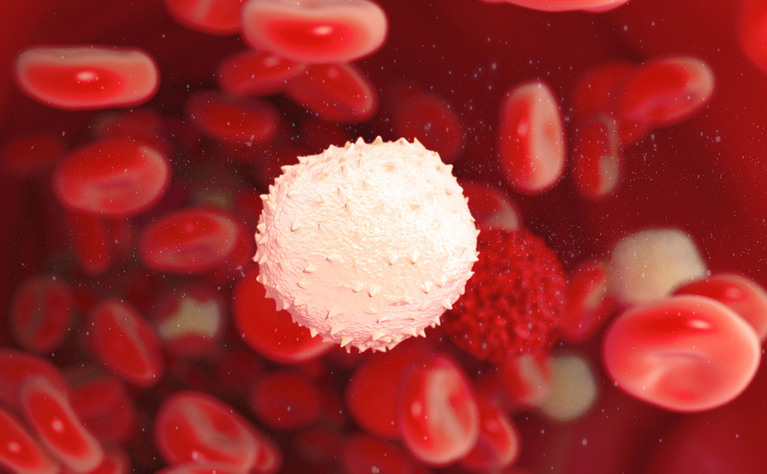
In lymphocytic colitis there is an increased number of lymphocytes (white blood cells) within the lining of the colon. Lymphocytes are part of the body’s defence system to fight infection and disease.
Collagenous colitis
In collagenous colitis, the lining of the colon develops a thicker than normal layer of a protein called collagen. There may also be an increased number of lymphocytes in the lining of the colon.
It is usually diagnosed through biopsies taken during an colonoscopy examination - a camera which is inserted into your rectum and colon. These biopsies are then examined at under a microscope to look for any changes to the bowel lining.
Unfortunately there is no known cure for microscopic colitis.
However, some people find that they can manage through changes to their diet and lifestyle without taking any medication, while others take medication to control the condition. Rarely some people do end up having surgery which removes all or part of their colon and/or rectum.


No one really knows what the exact cause of microscopic colitis is. The cause is often put down to a number of factors including:
It is also believed that some medications - such as aspirin, heartburn drugs and certain antidepressants can increase your risk of getting microscopic colitis.
Scientists continue to carry out research into the causes.
Microscopic colitis is generally diagnosed in people aged between 50-60, however you can be any age. It is more common in women. It is estimated around 2-3 people in every 10,000 have microscopic colitis.
People with microscopic colitis often go through periods of flare-ups where they have severe symptoms and periods where their symptoms are more mild or non-existent. Someone with the disease who isn’t displaying any symptoms is known to be in remission.
People who are diagnosed with microscopic colitis often wonder if there is a risk of it developing into the more severe forms of IBD - ulcerative colitis and Crohn’s disease - in the future. There appears to be a very small risk of this happening.
If you take steroid-based medication to help control your microscopic colitis then long term use could result in a weakening of your bones (osteoporosis).