Name: Seb Tucknott
Year of Birth 1986
Lives: Brighton, UK
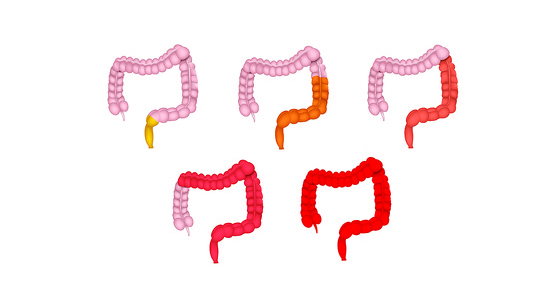
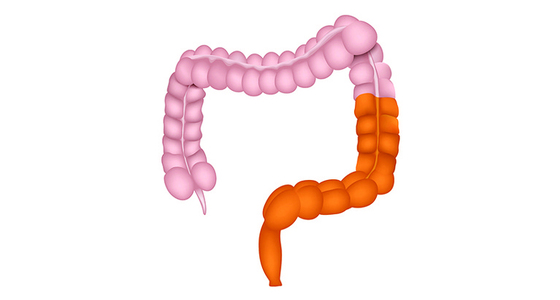
Type of IBD: Originally diagnosed with pancolitis, now proctosigmoiditis
Diagnosis Date: April 2008
Symptoms at Diagnosis: Bloody diarrhoea, weight loss
The first symptoms of my colitis happened on Easter Saturday - March 22, 2008. That day was the first time I noticed blood when I went to the toilet. I was taking photographs at a swimming meet in Reading for work and when I went to the toilet there it was, blood on the toilet paper when I wiped. At the time I didn’t think anything of it. I didn’t realise that from then on my life was going to dramatically change. I just chucked the paper into the toilet bowl, flushed and carried on with my day.
The blood continued for several days after I returned home to Brighton, and then I started experiencing bloody diarrhoea too. I went to my GP and was told I had haemorrhoids, was given some cream for them (without an examination being done) and was sent on my way. I felt the diagnosis was wrong so I didn’t use the cream and carried on for the next few days hoping the diarrhoea would go away. But it didn’t. It got worse. A lot worse.
So, back to the doctor I went. This time a different doctor took me more seriously. I was given steroid enemas, a referral to a gastroenterologist for six weeks’ time and a blood test. By now I had started Googling and I was pretty sure I had ulcerative colitis and as the days passed while I waited for my referral my symptoms got worse and worse. But, I refused to let them get in the way. I’d played every match that season for my football team, Portslade Athletic, and it was the last two games of the season. I wasn’t going to miss them for anything. Before the first game I told my manager I might need to rush off into the bushes to go to the toilet, but not to sub me as I’d be back! I made it through the game without needing the toilet but thought I was going to black out at one point. At half time in the final game of the season I was desperate and rushed off to the toilet while all my team-mates had the ‘half-time talk’. By the time I’d finished doing my business everyone was back on the pitch and waiting for me, slightly embarrassing! My efforts were worth it though, we won both games and I was awarded player of the season.
First symptoms started
Admitted to hospital and sigmoidoscopy showed colitis
Started taking azathioprine
Stopped 6 months later
First snowboarding trip since diagnosis
Finally managed to come off steroids
Put on antibiotics and one of worst flares started
Back on steroids
Started 6-Mercaptopurine alongside the steroids
London Olympics inspired me to take up athletics
Saw acupuncturist and changed diet
Stopped taking steroids and 6-Mercaptopurine
Became Sussex Champion in 200m and 400m
Started making other diet and lifestyle changes
Colonoscopy showed mild to moderate proctosigmoiditis
Colonoscopy shows clinical remission
Over the next few days my symptoms became even worse and I ended up going to A&E. A paediatric doctor examined me (he had a giraffe stethoscope!), despite the fact I was an adult. He asked if I had a fever - I said no - and he said it can’t be colitis as it always presents with a fever. He also concluded I had haemorrhoids (again no examination) and sent me on my way.
By now I was really struggling. I was going to the toilet every half hour. I wasn’t eating or drinking as everything was just going through me and I had lost 10kgs in 2 weeks. I couldn’t cope and went back to A&E. Finally a doctor carried out a digital examination. They didn’t find any haemorrhoids but did find mucous. I was so relieved that someone had finally found something. I was sent to an assessment ward. My blood was taken (using a cannula and a syringe because I was so dehydrated), was given a glucose drip and I spent the night there. I couldn’t sleep. I just walked up and down dragging my drip around. In the morning I was given an enema ready for a sigmoidoscopy and was moved on the gastroenterology ward.
The moment the pictures of sigmoidoscopy came up on the screen I knew I had ulcerative colitis. I could see the inflammation; it looked just like the pictures I had seen on Google. My colon was in a bad way and I was told I may need to have emergency surgery. They took biopsies and I was taken to the recovery ward. A male nurse came over to talk to me, but I just burst into tears. So many emotions came flooding out - relief they had found what was wrong with me and that I was going to looked after but also fear about the future. I’d read so many negative things about UC online and I was scared. I didn’t think I would be able to enjoy any of the things I had before again. Of course, I now know that’s not the case, but no-one told me that at the time.
There was no room for me on the gastroenterology ward so I spent an interesting 24 hours on the amputee ward instead! I was given IV steroids, an X-ray to check for blockages and afterwards was taken off nil-by-mouth. I had a sandwich...which tasted amazing! When the staff shift change took place I was placed back on nil-by-mouth though as the new consultant thought I did have a blockage after all and was given an NG tube (which was a pretty unpleasant experience). This was now April 8 and shortly after the NG tube was fitted Liverpool were playing Arsenal in the Champions’ League. I watched it from my bed and it was a nail-biting match. Afterwards the nurses came to do their rounds and they were worried about me as my heartrate was so high. I had to reassure them that it was just because of the football!
I managed to sleep a bit that night and when I woke up my arm felt strange. I didn’t really look at it but told the nurse that something didn’t feel right. Turns out the cannula had come out of my vein and had been pumping glucose and IV steroids straight into my arm tissue, and it was huge! For the next five days I was left with a very inflated arm! Despite this the steroids seemed to be working and my diarrhoea had started to lessen.
When the next consultant came on duty a short time later they decided I didn’t have a blockage after all and they took the NG tube out.
In total I spent nine days in hospital. I was sent home with Pentasa (mesalazine) and oral corticosteroids (Prednisolone) and an appointment to see a gastroenterologist. The gastroenterologist talked to me about what life with colitis would be like. He told me I would probably not be able to exercise as much. Being active has always been a big part of my life. I love playing football, mountain biking, trials riding, skiing, snowboarding, so this was a big blow. I was referred for a colonoscopy. The result was severe pancolitis. No wonder I had been bleeding so badly, they said.
After being back at home for a while, and once the diarrhoea and bleeding started to settle down, I tried to taper down my steroids, as directed. I was taking eight tablets (40mg) a day but every time I went below 20mg my symptoms would get worse and I would have to increase the dose a bit more.
In August 2008 Emily and I got together. At first I didn’t really talk to her about the effect my UC had on me. I made out that it was under control. We would go for creamy Italian dinners, cocktails in trendy bars, share a bottle of wine in front of a film. None of these were good for my colitis, but I still tried to hide it. The truth was that there were several occasions when I had an accident walking Emily home at night or while driving to meet her. It’s was only years late that I found the courage to tell her this. I can laugh about it now, but at the time it was devastating.
In January 2009 I was still struggling to cut down on the steroids. At this point my steroid ‘moon face’ was well established, as was an outrageous appetite (mostly for things that weren’t good for me!). I started taking azathioprine alongside the steroids. Around this time I also went on my first holiday with Emily (and her friends), a snowboarding trip to Les Deux Alpes. I felt awful the whole time but I was determined to snowboard, the consultant’s words about not being able to exercise as much ringing in my ears. And I did join in. I also started playing football again around that time. But, taking the azathioprine just didn’t make me feel like myself. I continued to take it for around six months but stopped as I still couldn’t taper off the steroids.
So I carried on with the steroids, a seemingly endless cycle of trying to drop the dose, my symptoms getting worse, and then upping the dose again. Then, towards the end of the year I suddenly managed it. I stopped taking steroids completely and for around nine months was just on Pentasa. There didn’t seem to be a reason why I’d suddenly managed it but it felt great to finally lose the moon face and drop some weight. It lasted for around nine months, but in June 2010 I got a tooth abscess which I had to take antibiotics for and one of my worst flares began. Out came the steroids again.
All the time that I’ve had colitis I have run my own company. This has been both a blessing and a curse - a blessing because it has given me flexibility when I haven’t been well to stay at home in the toilet or go home for an afternoon nap because I was feeling so fatigued, but a curse because it causes me a lot of stress. Some of the worst flares I’ve had have been triggered by a stressful event - and all these stressful events have been work related. I flared badly after my business partner left the company, when I had to make several people redundant, when I haven’t been able to pay staff and when there was too much work to do (or too little). I’ve now learnt a lot of coping strategies to help me deal with the stress.
In March 2011 Emily and I got married in an idyllic wedding in the French Alps. Just before the ceremony I did need to make a quick toilet pit stop in a mountain side bar. My best man worried that Emily was going to arrive at the ceremony and I wouldn’t be there, but thankfully I made it back and I survived the rest of the day. When I look back on photos from the day now it’s so obvious that I was taking steroids at the time - the moon face so prominent.
By now I knew that stress was a huge trigger for making my symptoms worse and I had discovered some other things too. I avoided eating tomatoes, salad leaves, grapes, and anything else with tough skins and seeds. I also knew that alcohol wasn’t good for me (though I still drank it a little). But, I still largely continued my life as it was. I had accepted this was how it was going to be. When I was diagnosed I was told they weren’t far off from finding a cure for colitis so I was happy to continue taking the medication until they did. But, the search for a cure continues and I’m not sure a cure is as close as was made out to me. In the summer of 2012, still struggling to keep my flares under control, my consultant added 6-mercaptopurine to the medications I was taking as he wanted me off the steroids (although I didn’t really feel the 6-MP did anything for me).
Then a cliché, life-changing moment happened. I’ve always enjoyed athletics (I competed when I was younger until I got Osgood-Schlatter disease in my knees which made it painful to train) and watching the London 2012 Olympics reminded me of how much I missed it. So I decided, there and then, that I was going to start training again. I joined Brighton Athletics Club and found I was still pretty good. My times weren’t bad and there was lots of room for improvement. At the same time I also found my colitis symptoms started to improve, and not just the toilet-related ones. My muscles and joints were aching less and I had more energy. My mother is Finnish and as my times steadily improved I decided I wanted to try to run for Finland. But, to compete at a national level I thought I would need to come off my steroid medication (although now I know this wouldn't have needed to be the case).
In November 2012 I went to see an acupuncturist who is a friend of my brother’s. He said he could help me with my symptoms. I have a science background and have never really been a believer in alternative medicine but my desire to get off the steroids was so great that I was willing to give anything a go. The treatment was incredibly relaxing and he also told me to stop eating gluten, dairy and nightshades if I wanted to really help myself. Again, I decided I had nothing to lose by trying it. Emily was already being very supportive in adapting the foods we ate to suit my colitis but when I told her I was no longer eating gluten, dairy or nightshades I remember her asking what we could actually eat. But, once she got used to the idea she embraced it fully. I continued with the acupuncture treatments for a while and the diet seemed to be having an effect.
In January 2013 I was able to come off the 6-mercaptopurine and steroids (and haven’t been back on them since), in May I became Sussex Champion in 200m and 400m and in July I went on a mountain biking holiday to the French Alps.
Sadly, I haven’t reached my goal of competing for Finland. Work and having a baby have got in the way. But, I’m still going to training (and I’m probably getting a bit old now anyway).
Since then I’ve done a lot of research into why giving up gluten, dairy and nightshades has worked for me. I now also limit the amount of grains, sugar and processed food I eat, I don’t drink any alcohol and try to only drink filtered water. I’ve also made a hundred or so other small changes to my life (such as practising mindfulness, having an air filter at home, using essential oils, taking a probiotic called Symprove, using a standing desk at work) which all play a part in helping me manage my colitis. You can read more about the things I do in this book I've written* (this is an affiliate link, and if you click on it we receive a commission when you buy. This doesn't affect the price you pay).
I’ve now also added another addition to my list - spending time with my little boy, Hayden. He was born in January 2015 in quite stressful circumstances (which caused my colitis to instantly flare to the point I had to use the sink in the labour room as a toilet while Emily was using the actual toilet). Whenever I’m feeling stressed or sad or angry spending just a few moments with him makes me feel great again.

I still have some bad days and I had a particularly bad flare in October 2013 when I was making some people redundant, but over the years I’ve learnt to manage my flares better and am incredibly strict with looking after myself when I feel like I’m heading towards a flare.
In January 2016 I had a colonoscopy. It was the first one since my pancolitis diagnosis and I was incredibly nervous. I was worried that all the changes I have done to my life hadn’t worked. Although I felt better and my symptoms had vastly improved I didn’t know what was going on inside me, and I was scared of what they might find. And, for the first few moments of the colonoscopy I thought the changes hadn’t made any difference. There was obvious inflammation in the rectum and transverse colon, but as the endoscope moved further up my colon and reached the transverse bend there was nothing - no ulcers, no inflammation. I came away with a diagnosis of mild to moderate proctosigmoiditis. To say I was elated is an understatement and when I told my family the results seeing how happy they were for me has made me even more determined to keep my new lifestyle up.
As the months passed I carried on making lots of small changes to keep my health in the best place possible. I started to feel better and better and would forget about my colitis for weeks, so much so that I was forgetting to take my Pentasa. Eventually I stopped taking this too. I felt great for around six months but then I had a flare. I was incredibly stressed at work and wasn’t sleeping. My diet had also slipped, I got a cold and my immune system was low. I was due to cycle the South Down’s Way (100 mile off-road cycle) for charity in 10 days’ time and I was worried I wouldn’t be able to make it through. However, I focused on my health by going to bed early, eating nutritiously and de-stressing and I made it through the flare and through the bike ride.
During that period I had a calprotectin test done, with a result of over 300. Six months later I had another and it was back down to 60. To make sure things were still OK my consultant was keen for me to have another colonoscopy. So in November 2017 I was back in the endoscopy unit, and again I was nervous. Having only recently been through a bad flare with a high calprotectin level I was sure that things wouldn’t look good, even though I was back to feeling great again. However, I couldn’t have been more wrong. Things looked even better than they had nearly two years previously. There was no sign of inflammation at all and I was told I was in clinical remission.
Starting IBDrelief
My experience inspired Emily and I to start IBDrelief in 2015 and in 2016 we launched the website that you are reading this story on. We wanted to try to improve the quality of information available for IBD patients and their families. It hasn't been an easy or straightforward journey, but IBDrelief and patient advocacy is now my fulltime job!
Then a couple of years later, during the pandemic, Emily and I split up. Although it was very amicable and we remain friends and colleagues it was still very stressful - but despite this my UC remained stable.
I can honestly say I have never felt as good as I feel now (even before my colitis), but life can be unpredictable and I know this doesn’t mean that things won’t change in the future. Right now though, I’m just enjoying every day while I can. I believe that by supporting my body to be in the best health it can possibly be I’ve helped my colitis to reach remission and am giving myself every opportunity to stay that way for as long as possible.